Cancer mortality rates have plunged, dropping one-third, since the 1990s, according to a recent report from the American Cancer Society.
The American Cancer Society estimates the number of new cancer cases and deaths in the United States annually, using the most recent data on population-based cancer occurrence and outcomes with data from central cancer registries and mortality data from the National Center for Health Statistics. Cancer is the second-leading cause of death in the United States, behind heart disease.
According to the latest data projections, 1,958,310 new cancer cases and 609,820 cancer deaths are expected in the United States in 2023. Many health experts have speculated that cancer mortality rates will rise in the years following the COVID-19 pandemic, as many Americans put off routine healthcare, including cancer screenings during the height of the virus and before vaccines were widespread. However, it will likely take many years to quantify the pandemic's true impact on cancer death rates.
The latest statistics show the cancer mortality rate has decreased continuously since 1991, with an overall drop of 33%. That's roughly 3.8 million cancer deaths avoided over the last three decades.
The findings are consistent with other reports showing improvements in cancer death rates due to better access to screenings and better treatments. Prior to the COVID-19 pandemic, data revealed cancer death rates were actually at their lowest since the 1990s. There are several reasons for this drop over time, according to the American Cancer Society.
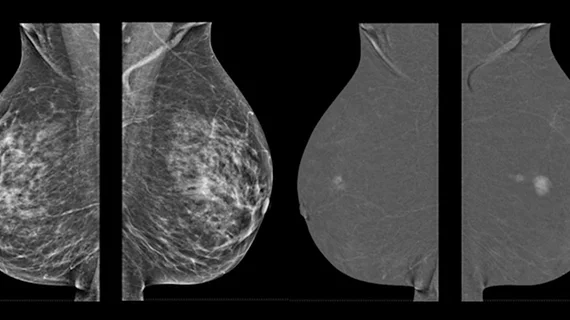
“This steady progress is because of reductions in smoking; uptake of screening for breast, colorectal, and prostate cancers; and improvements in treatment, such as adjuvant chemotherapies for colon and breast cancers,” wrote first author of the report Rebecca L. Siegel, MPH, senior scientific director, cancer surveillance research, et al.
Additionally, advancements in targeted treatment and immunotherapy have accelerated progress in lung cancer mortality, as well as leukemia, melanoma and kidney cancer.
Despite some progress among certain cancers, there are others that are not seeing drops in mortality and incidence rates. In particular, rising incidence for breast, prostate and uterine corpus cancers are of concern. In addition, these cancers have a wide racial disparity in mortality “and are amenable to early detection,” the report stated.
“Expanding access to care and increasing investment for the broad application of existing cancer control interventions and for research to advance treatment options and develop successful interventions to reduce inequalities would help mitigate disparities and accelerate progress against cancer,” the report stated.
While the report can portray a reasonably accurate projection of the “contemporary cancer burden,” the estimates are model-based, three-year (mortality) and four-year (incidence) projections that should not track trends over time. This is because new methodologies regularly come into play that use improved modeling techniques, including the 2021 estimates. Models can also only account for trends through the most recent data year, which is 2019 for incidence and 2020 for mortality. That means the current figures do not reflect the changes and reductions to access to healthcare due to the COVID-19 pandemic. Additionally, the model is sensitive to steep or sudden changes in the data.