Eyes are, as the saying goes, a gateway to the soul—but recent research shows they may be key in improving diagnosis of and treatment of schizophrenia. RETeval, a handheld device used by optometrists to track electrical activity from the retina, may help detect abnormalities related to schizophrenia.
“Since the retina is part of the nervous system, what is happening in the retina is likely reflective of what is occurring in the brain,” said Steven Silverstein, PhD, professor of psychiatry at Rutgers Robert Wood Johnson Medical School and director of research at Rutgers University Behavioral Health Care (UBHC), in a prepared statement. “For example, we know that certain changes in the retina, like thinning tissue [due to cell loss] or weakening electrical activity, occur alongside loss of brain tissue and reduced brain activity in patients with neurological disorders like multiple sclerosis and Parkinson’s disease. We and other researchers are now investigating whether retinal changes are related to brain structure and function changes in schizophrenia.”
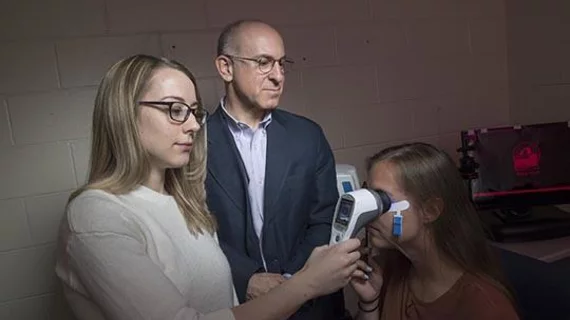
The study, published in the May issue of Journal of Abnormal Psychology, included 25 individuals with schizophrenia and 25 unaffected people. Researchers tested the participants with the RETeval device, which flashed different colored lights into the eye. An electrode recorded the retina’s activity.
“While the portable device clearly distinguished people with schizophrenia from those without a psychiatric diagnosis, it’s too soon to call this a diagnostic tool,” said lead author Docia Demmin, a graduate assistant in UBHC’s Division of Schizophrenia Research. “However, since every prior study has found that people with schizophrenia exhibit reduced retinal wave forms and slowed retinal responses, our research shows that we are closing in on an accurate test that is faster, less invasive, inexpensive and more accessible to patients.”