Two deaths of participants in a new experimental drug treatment trial targeting Alzheimer’s disease has raised concerns about the treatment's safety, but the drugmaker Eisai has denied the link.
Eisai is a Japanese pharmaceutical company that develops and manufactures the Alzheimer's targeting drug Lecanemob, and has worked with American biotechnology company Biogen since 2014 on the development and commercialization of Alzheimer's Disease treatments.
Researchers on the drug trial published their most recent findings in the New England Journal of Medicine (NEJM), reporting some promising results. The drug treatment, called lecanemab, is a humanized monoclonal antibody that binds with high affinity to soluble amyloid-beta (Aβ) protofibrils. Amyloid removal has been shown in some cases to slow the progression of Alzheimer’s, though there are currently few options to alter the underlying disease of Alzheimer’s.
Participants who received the treatment showed 27% less cognitive decline compared to those who received a placebo. This impact has created buzz around the potential of lecanemab to effect Alzheimer’s treatment. However, the second death raised alarm bells about the safety of the treatment should it get approval for use in the market.
Eisai denied the deaths were caused by lecanemob.
"The two cases on lecanemab occurred in the open-label extension study. Both cases had significant comorbidities and risk factors including anticoagulation contributing to macrohemorrhage or death," the company said in a statement. "Therefore, it is Eisai’s assessment that the deaths cannot be attributed to lecanemab."
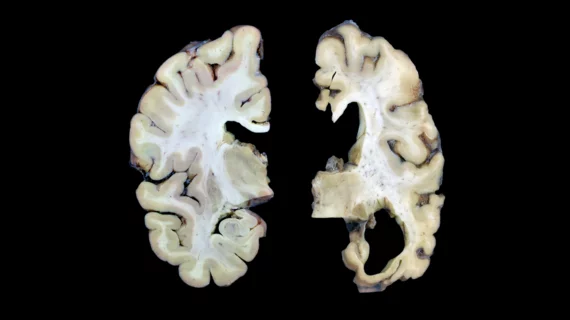
The second death that may be linked to lecanemab was first reported by Science, which obtained an unpublished case report of the trial findings. The death was of a 65-year-old woman who died of a brain hemorrhage and was receiving Alzheimer's treatment, including infusions of the antibody as part of the trial. She then suffered a stroke and “a type of swelling and bleeding previously seen with such antibodies, which bind to and remove forms of amyloid-beta, a protein widely theorized to cause Alzheimer’s,” Science reported.
The patient's husband requested an autopsy, and the Northwestern neuropathologist who conducted it, Rudolph Castellani, told Science the case was "very dramatic."
“It was a one-two punch,” Castellani said. “There’s zero doubt in my mind that this is a treatment-caused illness and death. If the patient hadn’t been on lecanemab she would be alive today.”
However, Castellani noted his comments were his personal opinion and were not reviewed or approved by Northwestern.
The first death was highlighted by Stat, which noted the death was flagged by an investigator for bleeding in the brain.
The study of the drug trial revealed that, after 18 months, lecanemab was associated with lower cognitive decline. However, a phase 2b, dose-finding trial involving 854 participants with early Alzheimer’s disease did not show a significant difference between lecanemab and placebo at the 12-month mark.
The findings come at a critical time as medicine continues to seek ways to treat the underlying Alzheimer’s disease and dementia. In the United States, 10,000 people turn 65 every day, and the aging population will have a huge impact on healthcare over the coming years as the baby boomer generation requires more long-term care––and more people are expected to have Alzheimer’s or dementia in the near future. Currently, more than six million people are living with Alzheimer’s in the U.S., and that figure is expected to reach 13 million by 2050, according to the Alzheimer’s Association.
Despite reports of two deaths possibly linked to the trials, NEJM researchers did not associate the deaths with this drug treatment.
“Deaths occurred in 0.7% of the participants in the lecanemab group and 0.8% of those in the placebo group,” wrote first author Christopher H. van Dyck, MD, of the Yale School of Medicine, et al. “No deaths were considered by the investigators to be related to lecanemab or occurred with [amyloid-related imaging abnormalities (ARIA)].”
The questions about the possible second death in the drug trials led The Lancet to publish an editorial about lecanemob as the U.S. Food and Drug Administration is expected to make an initial decision about the drug’s approval by Jan. 6, 2023.
“Incidence of amyloid-related imaging abnormalities (ARIA), an adverse event associated with anti-Aβ antibodies and which manifests as oedema or microhaemorrhages, occurred in 21% of the lecanemab group; most cases were asymptomatic and detected incidentally,” The Lancet editorial wrote. “However, reports of a second death in the ongoing open-label extension phase of the study—possibly linked to co-administration of the thrombolytic drug alteplase—have heightened concerns about lecanemab's safety in patients taking blood-thinning drugs.”
The journal noted that the results were welcome news, but the actual impact may be low, and there are remaining concerns and questions about lecanemob’s ability to hold up to all its promises as a breakthrough treatment.