Humana is launching new partnerships in four states to better care for its Medicare Advantage and commercially insured members who have kidney care.
The health insurer, based in Louisville, Kentucky, has teamed up with Monogram Health, a personalized kidney services company, and Somatus, a provider of value-based kidney care, for its new programs. The agreements with the two companies will provide care coordination for Humana’s members affected by kidney disease, aiming to improve their quality of life and health.
Specifically, Monogram Health will serve Humana members in Louisiana and Mississippi, while Somatus will provide care in Georgia and Virginia. The services by Somatus will be available to eligible Humana members beginning Jan. 1, 2020, while Monogram Health’s program is already available.
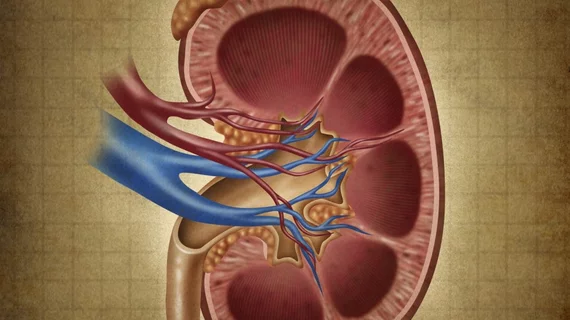
Chronic kidney disease impacts a person’s ability to properly filter blood, contributing to dangerously high levels of waste and fluid. The disease impacts more than 30 million Americans, according to the Centers for Disease Control and Prevention, and many are undiagnosed. Without proper care for the complex condition, those suffering from chronic kidney disease can see their health outcomes and symptoms worsen quickly.
“Through this collaboration, we will strengthen care coordination for Humana members with kidney disease. Our partnerships will offer customized care options and will empower patients with education and engagement tools to better manage their condition,” William Shrank, MD, MPHS, Humana’s chief medical and corporate affairs officer, said in a statement. “This multidisciplinary approach will focus on detecting kidney disease earlier, slowing disease progression, and utilizing therapies that enable members to receive care in the convenience of their own home.”
The launch of the programs by Humana comes at a time when kidney care has gained more national interest, with the Trump administration overhauling Medicare payment methodologies to provide better options for kidney care patients, including offering more services that can be performed at home.
Similarly, Humana’s services in the new programs will include teams from the two companies comprised of nephrologists, nurses, dietitians and social workers who will coordinate care with a member’s primary care physician and nephrologist, provide in-home health and medication assessments, offer patient education about treatment options like home dialysis, and give emotional support to members through counseling.
“Humana is pleased to be able to offer our members with chronic kidney and end-stage renal disease a range of specific care management services to meet their unique health needs and help them spend more time at home than at a clinical care facility,” said Susan Diamond, Humana’s Segment President, Home Business. “This is a holistic, comprehensive approach to care for members with late-stage kidney disease. Through these agreements, Humana is proud to deepen our longstanding commitment to improve the patient experience and health outcomes, while reducing the cost of care.”