Ohio Attorney General Dave Yost has taken aim at pharmacy benefit managers (PBMs), including Express Scripts and Cigna, for allegedly illegally driving up drug prices.
According to Yost, the PBMs––which are often dubbed the middle men of the healthcare industry, helping negotiate price rebates between pharmacies and drug manufacturers––used a a little-known, Switzerland-based company that drove up drug prices and pushed the higher costs onto patients, including for life-saving drugs such as insulin.
“Medications shouldn’t cost an arm and a leg, metaphorically or literally,” the attorney general said. “Insulin is just a symptom of the problem; PBMs are the disease.”
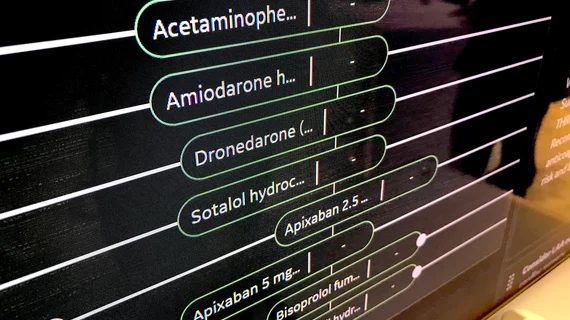
According to Yost, Express Scripts engaged in “a complex ‘pay-to-play’ rebate system that, perversely, pushes manufacturers to increase drug prices in order to be placed on, or receive, preferred placement on PBM formularies.” The company has relied on its market dominance to push the drug pricing scheme, rather than bring down costs for customers as it promises in its marketing, Yost stated. The biggest three PBMs, CVS-owned Caremark, Express Scripts and United Health-owned OptumRx, control 75% of the market, giving them a huge amount of power to control prices, Yost alleged.
“PBMs are modern gangsters,” Yost said in a statement. “They were designed to protect and negotiate on behalf of employers and consumers after Big Pharma was criticized for overpricing medications, but instead they have absolutely destroyed transparency, scheming in the shadows to control drug prices on all sides of the market.”
“The savings that PBMs claim from the inflated list prices are illusory,” read a statement from Yost’s office.
Yost, who filed the lawsuit in Delaware County Common Pleas Court, has argued the case is different than previous lawsuits that have come before because it only targets the PBMs, rather than including pharmacies or manufacturers being “strong-armed” by the PBMs. The suit alleges violations of the Valentine Act, Ohio’s antitrust law, which prohibits price fixing, controlled sales and other agreements that restrain trade and hurt competition.
Express Scripts has seemingly become the ire of Yost, who called out the company for creating “a group purchasing organization,” dubbed Ascent Health Services, in 2019 that would take over the company’s pricing and rebate negotiations with drug manufacturers. The company created Ascent at a time when PBMs were under fire for their role in driving up drug prices. However, Express Scripts offered Prime Therapeutics ownership in Ascent and relocated Ascent’s headquarters to Switzerland, effectively hiding its actions and “concealing its ongoing pricing and rebate scheme,” according to Yost.
The lawsuit alleges Ascent has been used by the two PBMs to “share pricing, discount and rebate information with each other and with Humana Pharmacy Solutions, an Ascent customer––driving drug prices up even higher.”
The lawsuit names Express Scripts, Cigna Group, Prime Therapeutics, Ascent, Humana Pharmacy Solutions, Humana and Evernorth Health (another subsidiary of Cigna) as co-defendants. The suit aims to halt the alleged secret and anticompetitive actions of the PBMs, as well as levying statutory fines and disgorging the companies from their allegedly ill-gotten profits.