Researchers in Israel are printing 3D models of brain tumors and connective tissues with synthetic blood vessels through which blood as well as anti-cancer agents can flow.
In this way the replicas can preview a given tumor’s reaction to specific therapies and combinations thereof.
The team expects the work, underway at Tel Aviv University, to personalize treatments patient by patient while simultaneously driving development of better-targeted drugs.
The achievement is described in a study published Aug. 18 in Science Advances.
Senior study author Ronit Satchi-Fainaro, PhD, and colleagues innovated the system to replace the use of 2D petri dishes for culturing cells of various cancers, followed by therapy experiments in mice.
This conventional approach yields only one usable anticancer drug out of every 10,000 tested, the authors note.
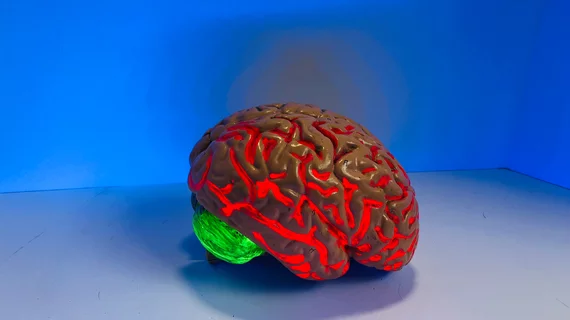
By contrast, the new technique 3D-prints exact replicas of specific glioblastomas from patients’ MRI scans.
Meanwhile the printing ink is a composite hydrogel—a bioink—grown in a bioreactor using cells extracted from the actual tumor.
The authors explain their system generates a closed circulatory system, which is how it allows blood cells, tumor cells and drug molecules to circulate and perfuse throughout the model.
“[O]ur perfusable 3D-printed model can be manufactured on demand to serve as a drug screening array for the evaluation of drug response, customized to each patient individually by including patient-derived tumor, stromal and immune cells in the 3D-bioink,” they comment. “The 3D tumor model can be printed rapidly and robustly, allow testing of several drugs or their combinations simultaneously with such perfusion system.”
In a news item posted by the university, Satchi-Fainaro says the system gives a treatment team about two weeks to test numerous therapies en route to identifying the most effective.
Noting that glioblastomas are among the most aggressive and thus deadliest brain tumors, the authors write:
[W]e postulate that our bioengineered, 3D-printed GB model could help in narrowing the ‘valley of death’ in drug development by advancing the preclinical studies and will revolutionize the way we treat patients with cancer by adequately mimicking the brain tissue and predicting the suitable clinical treatment to each person, which has special importance in tumors with short-term survival like glioblastoma.”